Have you ever wondered how doctors repair the slippery, shock-absorbing cartilage in your knees—a tissue so stubbornly resistant to healing that even paper cuts heal faster? Unlike skin, cartilage lacks blood vessels, making self-repair nearly impossible. For decades, orthopedic surgeons relied on microfracture surgery—a “drill-and-hope” approach similar to filling a pothole with gravel.
Let’s dive into this—and meet patients like Sarah, a 28-year-old soccer player, describes her post-microfracture experience: “After surgery, I felt hopeful. But 18 months later, my knee locked up like a rusty hinge. Squatting felt like grinding sandpaper.” Her story underscores a harsh truth.
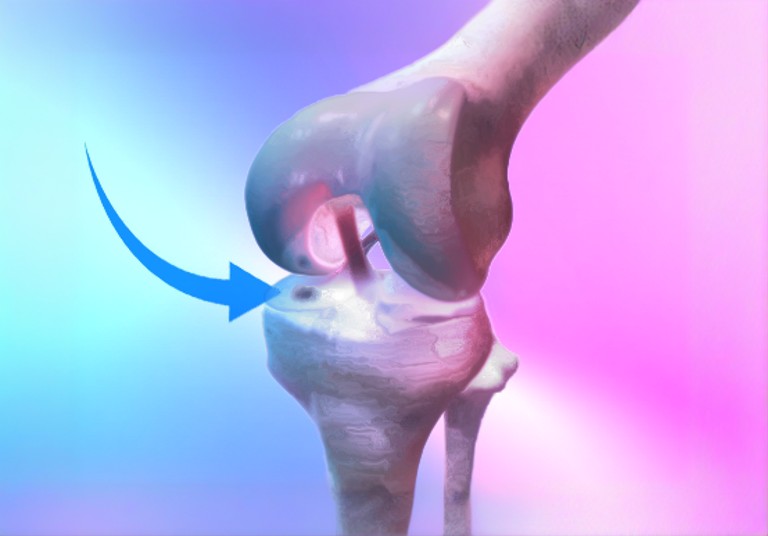
Microfracture: The “Quick Fix” That Often Fails
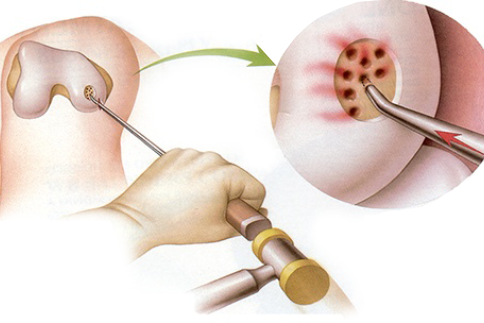
How It Works: Surgeon’s drill tiny holes (creating small fractures) into subchondral bone, releasing stem cells and blood to form a repair patch. The catch?
This patch is fibrocartilage—a “duct tape” tissue that’s stiffer and less durable than the natural hyaline cartilage lining our joints. Microfracture surgery is the IKEA assembly of cartilage repair—simple, affordable, but not built to last.
- Pros:
- Minimally invasive, 6–8 week recovery (Chung et al., 2023).
- Low cost, often covered by insurance.
- Why it falters:
- Fibrocartilage lacks the smooth, glassy surface of native cartilage, leading to friction and early arthritis (Boden, 2024).
- Up to 30% of patients develop subchondral cysts or bone hardening beneath the repair site, causing chronic pain (Zheng et al., 2025).
- For defects larger than 2 cm², failure rates skyrocket (Han et al., 2021).
Who It’s For: Older patients with small defects or those delaying joint replacement.
Sarah’s story is typical: After microfracture, she initially felt relief, but within 18 months, her knee stiffened.
OATS: The ‘Gold Standard’ for Cartilage Repair
OATS skips the duct tape and instead transplants living cartilage plugs from non-weight-bearing areas of the joint. These plugs contain both hyaline cartilage and underlying bone, seamlessly integrating into the defect.
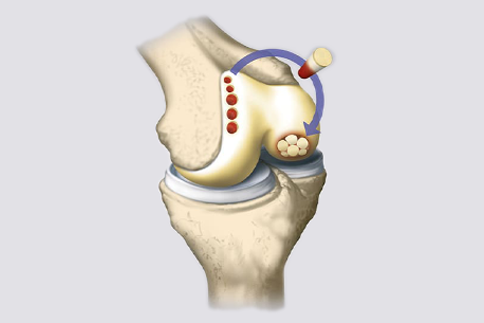
- Why OATS wins:
- 85% of patients return to sports within a year (Ballal et al., 2023).
- Less long-term arthritis risk—Hyaline cartilage has superior biomechanical properties for load bearing and stress distribution. (LaPrade et al., 2021).
- Lower revision rates: Only 8% of OATS patients need follow-up surgery vs. 22% for microfracture (Muthu et al., 2023).
Jake, a 32-year-old climber, underwent OATS after a talus cartilage injury. “Six months post-op, I was back on the wall. It’s like my ankle never broke.”
- But OATS isn’t perfect:
- Effective only for defects <3 cm² (Redondo et al., 2018).
- “Donor site morbidity” can leave new holes in healthy cartilage.
Who It’s For: Active patients under 50 with focal defects.
The Cartilage Repair Revolution: 3D Printing, Stem Cells, and CRISPR
While OATS is a leap forward, researchers are now chasing true regeneration—rebuilding cartilage that’s indistinguishable from the original. Here’s the cutting edge:
- 3D-Bioprinted Cartilage
Imagine printing a knee meniscus layer-by-layer using “bioinks” of stem cells and collagen. Teams like Zheng et al. (2025) have created hydrogel scaffolds that mimic cartilage’s squishy texture while guiding cells to grow into organized tissue. Early trials show these constructs integrate better than microfracture’s fibrocartilage mess. - Stem Cell “Cocktails”
Researchers are mixing mesenchymal stem cells with molecules like kartogenin (KGN), which acts like a “chondrocyte GPS” to steer stem cells into becoming cartilage cells (Zheng et al. (2025)). One trial saw 70% defect filling in 6 months—double microfracture’s results. - Acellular Scaffolds
The Agili-C scaffold, made from coral-derived aragonite, tricks the body into regenerating cartilage without foreign cells. Think of it as a biodegradable honeycomb that cells colonize naturally (Zheng et al. (2025)). - Gene Editing and Ultrasound
CRISPR is being tested to tweak cells’ genetic code, boosting collagen production. Meanwhile, low-intensity ultrasound pulses stimulate cartilage growth—like a cellular pep talk (Zheng et al. (2025)).
Who Gets Which Treatment?
- Microfracture: Best for older patients, small defects (<2 cm²), or as a bridge to delay joint replacement.
- OATS: Ideal for young athletes with focal defects.
- 3D Printing/Stem Cells: On the horizon for complex or large lesions.
The Future: A World Without Arthritis?
The shift from microfracture to OATS mirrors medicine’s broader move from “repair” to restoration. Yet the holy grail remains: regrowing hyaline cartilage that lasts a lifetime. As Dr. LaPrade notes, “In 10 years, we might combine 3D-printed scaffolds with gene therapy to make joints better than new.”
Comparative Snapshot
| Factor | Microfracture | OATS | 3D Printing/Stem Cells |
|---|---|---|---|
| Defect Size | <2 cm² | <3 cm² | Any size (experimental) |
| Durability | 2–5 years | 10+ years | Potentially lifelong |
| Best For | Older adults | Young athletes | Complex cases |
| Cost | Affordable | Expensive | Experimental (trials) |
Expert Tip: “Match the treatment to your lifestyle. A 50-year-old gardener might opt for microfracture, while a 25-year-old runner should push for OATS.” — Dr. LaPrade
FAQs
Q: Will I need a knee replacement later?
A: OATS delays replacement by 10–15 years; regenerative therapies aim to prevent it entirely.
Q: Are stem cell therapies safe?
A: Early data is promising, but risks include infection and inconsistent results (Focşa et al., 2024).
Q: Is gene editing FDA-approved?
A: Not yet—CRISPR is still in trials but could revolutionize care by 2030.
Food for Thought:
If we can 3D-print cartilage, will joint replacements become obsolete? And could athletes one day “upgrade” their cartilage to be more resilient? The race to conquer arthritis is just getting started.
For a broader perspective on knee pain, including how issues might stem from unexpected areas, check out our article Is That Knee Pain Actually Coming From Your Spine? What Most Doctors Miss. This piece delves into the intriguing connection between spinal health and knee pain—a reminder that sometimes, the answer lies well beyond the joint.
Drop a comment below—I’d love to hear your questions, stories, or wild predictions about the future of “bionic” knees!
Let’s keep the conversation moving—just like healthy cartilage should. 😉