Maria, a 42-year-old teacher, received a breast cancer diagnosis. Her initial biopsy suggested her tumor was HER2-negative, a result that would have excluded her from targeted therapies. But her oncologist, ordered a second test—HER2 FISH—that revealed a hidden truth: Maria’s cancer cells were flooded with HER2 genes. “It was like finding a secret door,” Maria recalls. “That test gave me access to drugs that saved my life.”
Maria’s story isn’t unique. For 1 in 5 breast cancer patients, HER2 status isn’t just a detail—it’s a lifeline.
What HER2 FISH Reveals
HER2 acts like a cellular “volume knob.” When amplified, it shouts growth signals, fueling aggressive tumors.
Enter FISH (fluorescence in situ hybridization), a molecular flashlight that illuminates HER2 gene copies inside cancer cells.
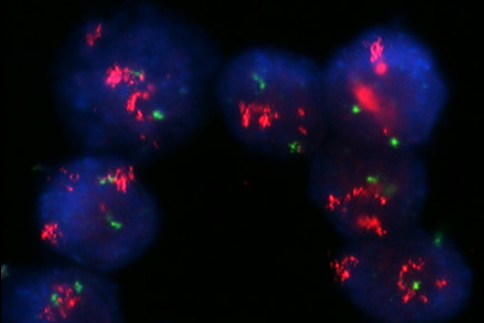
- How it works: FISH uses fluorescent probes to tag HER2 genes (pink) and their control chromosome (green). Under a microscope, technicians count the signals:
- >2.2 HER2/control ratio = Positive (targeted therapy works).
- <1.8 = Negative.
- Gray zone (1.8–2.2) = “Genetic limbo,” requiring deeper analysis (Aznab et al., 2022).
The Diagnostic Dilemma: When IHC Isn’t Enough
Immunohistochemistry (IHC), the cheaper, faster cousin of FISH, stains HER2 proteins. But it’s prone to ambiguity—like judging a painting in dim light. For IHC 2+ cases (“maybe positive”), FISH is the tiebreaker.
Key data:
- 15–20% of IHC 2+ tumors are HER2-positive by FISH—patients who’d miss life-extending drugs without retesting (Stenehjem et al., 2014).
- FISH accuracy: 98% vs. IHC’s 80–85% (Chaleshtori et al., 2020).
The Challenge: When Genes Play Hide-and-Seek
Even FISH has puzzles. Take polysomy 17, where the control chromosome multiplies, skewing ratios. New guidelines recommend dual probes or alternative controls to avoid misclassification (Holzschuh et al., 2017).
Patient impact: In 2021, guideline updates reclassified 4–7% of “negative” tumors as HER2-positive, qualifying thousands more for targeted therapies (Press et al., 2019).
From Diagnosis to Survival: The Treatment Revolution
HER2-positive cancers were once the worst prognosis. Today, drugs like trastuzumab (Herceptin) and pertuzumab silence HER2’s roar, boosting survival rates by 30–50% (Chorn, 2006).
The Future: CRISPR, AI, and Liquid Biopsies
Speculative scenario: By 2030, AI could analyze FISH slides in seconds, while CRISPR-based therapies edit HER2 genes preemptively. Researchers are even exploring “liquid FISH” to detect HER2 amplification via blood tests—no biopsy needed (Horii et al., 2014).
Closing: A Call for Clarity
“Knowledge is power, but accuracy is survival,” says Maria, now cancer-free. As science evolves, so does our ability to decode cancer’s secrets. For patients, that means hope isn’t a maybe—it’s a ratio, a fluorescent signal, a second chance.
Key Takeaways
- FISH fixes IHC’s blind spots, ensuring no patient misses targeted therapy.
- Guideline updates matter: Tiny ratio changes = life-changing treatments.
- The future is bright: Automation and AI promise faster, cheaper FISH (Öhlschlegel et al., 2013).




